Chronic kidney disease (CKD) affects numerous pets, but when detected in the early stages, the condition can often be effectively managed to increase a pet’s quantity and quality of life. Our Juanita Hills Animal Hospital team wants all our patients to enjoy a long, happy life, and we answer your frequently asked questions (FAQs) about CKD.
Question: What is chronic kidney disease in pets?
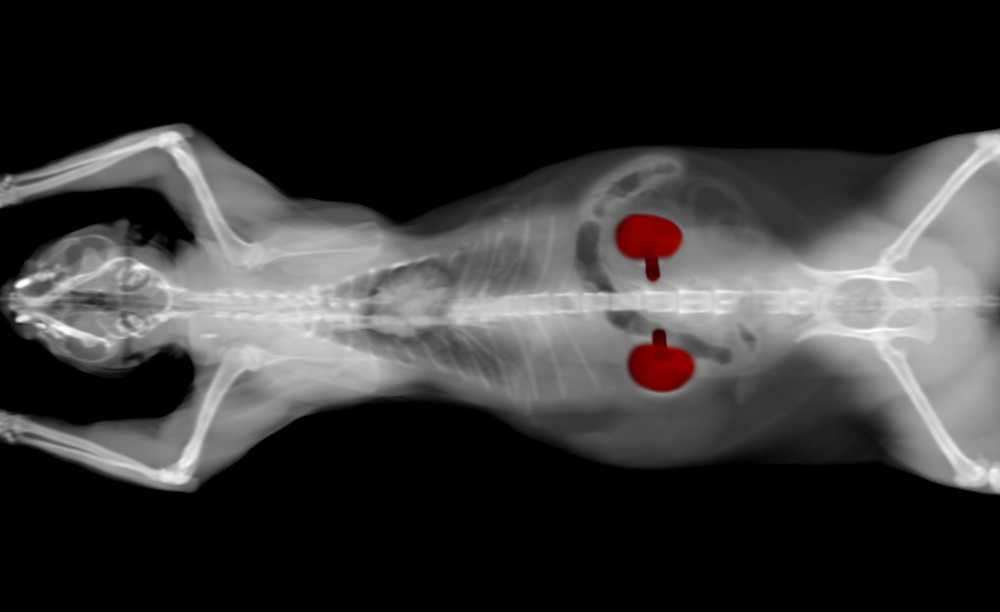
Answer: CKD is the persistent decline in kidney function. Because the kidneys play a vital role in the body’s numerous systems, their health is essential to avoid these complications:
- Toxin accumulation — The kidneys’ numerous filtering units (i.e., nephrons) are responsible for removing toxins and waste from the body. When the kidneys don’t function properly, toxins accumulate.
- Protein loss — The kidney filtration system normally preserves important proteins. However, when CKD occurs, the system is damaged, and protein is lost in the urine.
- Elevated blood pressure — The kidneys are responsible for regulating blood pressure, and kidney dysfunction leads to hypertension, which can further damage these organs.
- Anemia — The kidneys produce erythropoietin, a hormone responsible for regulating red blood cell (RBC) production. CKD causes decreased erythropoietin production, which leads to anemia.
- A pH imbalance — The kidneys typically keep the body’s pH in a narrow range, but CKD inhibits this regulation, interfering with many metabolic processes.
- Electrolyte and mineral disturbances — The kidneys are responsible for balancing electrolytes, such as sodium and potassium, and minerals, such as calcium and phosphorus. Kidney dysfunction leads to imbalances, resulting in significant complications throughout the body.
Q: What causes chronic kidney disease in pets?
A: CKD typically affects older pets. Researchers believe the condition occurs because the kidney tissues are wearing out. However, age is not the only factor that affects your pet’s CKD risk, and your four-legged friend is predisposed to developing this disease if they have one of the following conditions:
- Infection — Prolonged or chronic kidney infections damage these organs, which can lead to CKD.
- Tick-borne disease — Tick-borne illnesses, such as Lyme disease and anaplasmosis, can cause kidney dysfunction.
- Toxicity — If a pet recovers from a toxicity that causes acute kidney disease, the resultant damage can lead to CKD.
- Dehydration — Maintaining hydration is extremely important for kidney health. Without proper perfusion, kidney tissue is damaged, leading to CKD.
Q: What are chronic kidney disease signs in pets?
A: Most pets don’t exhibit signs in the disease’s early stages, making CKD diagnostic screening tests extremely important. As a pet’s kidney function deteriorates, signs include:
- Decreased appetite and weight loss
- Lethargy
- Vomiting
- Drooling
- Increased thirst and urination
- Bad breath
Q: What are the usual screening tests for chronic kidney disease in pets?
A: During your pet’s annual wellness examination, our Juanita Hills Animal Hospital team will perform tests to evaluate your pet’s kidney function. CKD diagnostic screening tests include:
- Complete blood count (CBC) — A CBC evaluates your pet’s white blood cells (WBCs), RBCs, and platelets. CKD causes a decrease in erythropoietin production, which leads to a low RBC.
- Creatinine — Creatine supplies energy to the muscles, and when this chemical is broken down, creatinine is produced. Healthy kidneys filter out creatinine, and elevated levels can indicate CKD.
- Blood urea nitrogen (BUN) — When the liver breaks down protein, the organ produces BUN as a waste product, which the kidneys typically filter. Elevated levels can indicate CKD.
- Urinalysis — The kidneys typically prevent protein loss, and CKD can lead to proteinuria (i.e., protein in the urine).
Q: Are these tests sufficient to detect chronic kidney disease in pets?
A: By the time creatinine and BUN levels increase, approximately 66% to 75% of functional kidney cells have been damaged. In addition, abnormal CBC and urinalysis test results can indicate conditions unrelated to CKD. Relying solely on these tests can delay a CKD diagnosis and treatment, negatively impacting your pet’s prognosis.
Q: Are new test options available to help detect chronic kidney disease in pets earlier?
A: In 2015, the symmetric dimethylarginine (SDMA) test became accessible to veterinarians at certain reference labs, and this diagnostic screening test is now widely available. SDMA is a more sensitive and specific test for kidney function than BUN and creatinine tests. SDMA can detect CKD when as little as 25% of functional kidney cells are damaged. To help detect early stage CKD, when the condition is easier to manage, the International Renal Interest Society (IRIS) recommends including SDMA, along with traditional diagnostic screening tests, when checking a pet for CKD.
Q: How often should my pet be screened for chronic kidney disease?
A: Adult pets should be screened for CKD once per year, when they have their annual wellness examination. Senior pets have a high CKD risk, and should be screened every 6 months.
Q: How does early chronic kidney disease diagnosis affect my pet’s treatment?

A: Pets affected by CKD are staged according to several factors, including blood creatinine and SDMA levels. Stages include:
- Stage 1 — These pets have a normal blood creatinine level and normal or mildly increased SDMA. Pets do not exhibit signs at this stage.
- Stage 2 — These pets have a normal or mildly increased creatinine level and mildly increased SDMA. If a pet exhibits signs, they are usually mild at this stage.
- Stage 3 — These pets have a mild to moderate increased creatinine level and a moderate to high SDMA increase. Pets usually exhibit mild to moderate signs at this stage.
- Stage 4 — These pets’ creatinine and SDMA levels are significantly elevated. Pets in this CKD stage have a high veterinary crisis risk.
The IRIS provides detailed treatment recommendations for each CKD stage. If your pet is in the early CKD stages, your veterinarian will likely put your furry pal on a special diet and ensure their hydration is maintained. If your pet has advanced CKD, your veterinarian will provide more aggressive treatment, including numerous medications to control secondary complications. In addition, they may recommend inserting a feeding tube to ensure your four-legged friend gets adequate nutritional support.
Schedule your pet’s routine wellness examination to have them screened for CKD. To ensure your furry pal’s kidneys are healthy and functioning well, contact our Juanita Hills Animal Hospital team.


















Leave A Comment